Susanna’s Cool Cancer Research Finds: July 2024
Every week, Dr. Susanna Greer, the V Foundation's Chief Scientific Officer, shares her cool cancer research finds on LinkedIn. Read more below to see highlights from the latest top finds!
July 2, 2024
Cancer research is for all
This week’s Cool Cancer Find is from the V Foundation Grantee Dr. Sidharth Puram, Division Chief of Head and Neck Surgery at Siteman Cancer Center. The Puram lab studies head and neck squamous cell carcinoma, (HNSCC), which is the sixth leading cause of cancer-related deaths and is particularly challenging to treat, especially for non-Hispanic Black patients. This aggressive cancer often spreads and returns after treatment, and the difference in outcomes between racial groups is significant.
 One focus of HNSCC research is why some people have a tougher time with this cancer than others. The differences are due to factors including access to good medical care, treatment plans, and support systems and also things like the genetic makeup of the tumors and the environments people live in.
One focus of HNSCC research is why some people have a tougher time with this cancer than others. The differences are due to factors including access to good medical care, treatment plans, and support systems and also things like the genetic makeup of the tumors and the environments people live in.
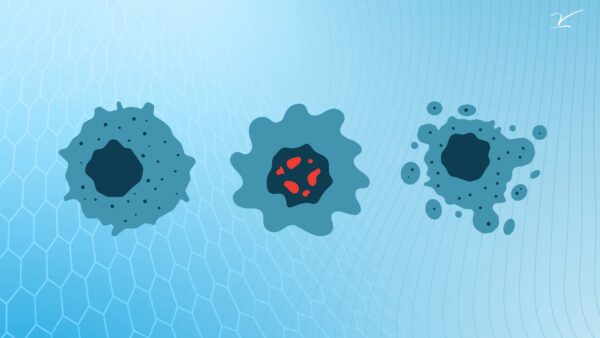
HNSCC is also tricky because the tumors are often very different from one another, even within the same patient. In this study, Dr. Puram and team used a technique called single-cell sequencing to look closely at HNSCC tumors. They found that the cancer cells at the edge of the tumors can change in a way that helps them spread to other parts of the body. This change involves the cells having characteristics of both epithelial (covering surfaces) and mesenchymal (moving around) cells.
By analyzing gene expression data and survival rates, the team discovered that non-Hispanic Black patients with these hybrid cells have a higher risk of death or cancer recurrence compared to non-Hispanic White patients.
 These findings further stress the need to consider both social factors, such as access to care and environmental stress, and biological differences, like genetic diversity, in cancer research. More diverse studies are essential to develop better treatments and improve outcomes for all patients, especially those from underrepresented groups. Research often doesn’t include enough patients from diverse backgrounds. This makes it hard to understand and address racial differences in cancer outcomes. More studies need to include Black patients and gather information about both their genetics and their social environments to find better ways to treat everyone.
These findings further stress the need to consider both social factors, such as access to care and environmental stress, and biological differences, like genetic diversity, in cancer research. More diverse studies are essential to develop better treatments and improve outcomes for all patients, especially those from underrepresented groups. Research often doesn’t include enough patients from diverse backgrounds. This makes it hard to understand and address racial differences in cancer outcomes. More studies need to include Black patients and gather information about both their genetics and their social environments to find better ways to treat everyone.
You can read Dr. Purham’s outstanding paper here: A hybrid epithelial/mesenchymal state in head and neck cancer: https://doi.org/10.1016/j.medj.2024.05.014 and follow the lab at https://oto.wustl.edu/people/sidharth-v-puram-md-phd/.
July 14, 2024
Our researchers don’t cut corners – they’re cutting edge.
This week’s Cool Cancer Find focuses on refining a cutting-edge cancer treatment called Adoptive T-cell transfer (ACT) therapy, where patients are given specially prepared T cells that can target and attack their tumors.
In ACT, T cells are extracted from the patient, genetically modified, or selected for their ability to recognize cancer cells, and then multiplied in the laboratory. These enhanced T cells are then infused back into the patient to help their immune systems fight their cancers better.
 This study from the V Foundation Grantee Dr. Chrystal Paulos Winship Cancer Institute of Emory University focuses on optimizing the preconditioning methods that prepare the patient’s body to receive these T cells, making the treatment more effective.
This study from the V Foundation Grantee Dr. Chrystal Paulos Winship Cancer Institute of Emory University focuses on optimizing the preconditioning methods that prepare the patient’s body to receive these T cells, making the treatment more effective.
Why is optimization so important? Effective preconditioning improves the likelihood that the adoptively transferred T cells will survive, proliferate, and effectively target cancer cells within the patient’s body. By creating a more supportive environment for the T cells, the chances of achieving a durable and effective anti-cancer response are significantly increased.
Said another way, Dr. Paulos demonstrates that preconditioning is crucial because it helps create a more favorable environment in the body for the infused T cells to survive to attack the tumor. These findings are significant as they can lead to improvements in ACT therapy, making it more potent for patients with challenging-to-treat cancers.
Why do I love this paper? Easy: these improvements will lead to a more potent and effective immune response against cancer, increasing the likelihood of successful treatment outcomes and long-term remission. Read this cool paper here: Distinct host preconditioning regimens differentially impact the antitumor potency of adoptively transferred Th17 cells (bmj.com) and find the Paulos lab at Chrystal M. Paulos, PhD | Winship Cancer Institute of Emory University.
July 18, 2024
Planting the seeds for a new treatment for childhood brain cancer.
This week’s Cool Cancer Find focuses on Medulloblastomas, the most common type of malignant brain tumors found in children. These tumors develop in a part of the brain called the hindbrain, which is responsible for controlling movement and balance. There are four main types of medulloblastomas, grouped based on their genetic profiles: SHH, WNT, Group 3, and Group 4. Among these, Group 3 is particularly dangerous. Children with Group 3 often have worse outcomes and the cancer tends to spread more quickly, making it a major focus for researchers like the V Foundation Grantee Dr. Michael Taylor and colleagues at the University of Toronto affiliated Hospital for Sick Children, Baylor College of Medicine, and in the Pediatric Neuro-Oncology Research Program at Texas Children’s Hospital.
The way Group 3 tumors develop is not well understood. To find out more, Dr. Taylor and team are studying the early development of the human brain. They have identified a type of cell called Protogenin (PRTG)-high stem cells. These cells play a crucial role in the early formation of the brain.
 Why does this matter? PRTG-high stem cells are like seeds that grow into different parts of the brain. In both normal brain tissue and Group 3 Medulloblastomas, these cells grow near immature blood vessels. This environment helps keep the stem cells alive and allows the tumor to grow. Normally, these PRTG-high cells stay in an immature state and gradually turn into different brain cells.
Why does this matter? PRTG-high stem cells are like seeds that grow into different parts of the brain. In both normal brain tissue and Group 3 Medulloblastomas, these cells grow near immature blood vessels. This environment helps keep the stem cells alive and allows the tumor to grow. Normally, these PRTG-high cells stay in an immature state and gradually turn into different brain cells.
In Group 3 Medulloblastomas, however, these cells remain in their immature state due to changes in their genetic makeup. This abnormal behavior helps the tumor to grow and spread. Just like a gardener provides a perfect environment for seeds to grow, the tumor cells create a nurturing environment for themselves by interacting with nearby immature blood vessels.
This research is significant because it offers a new way to treat a particularly aggressive type of brain tumor in children. By understanding and targeting the specific cells that drive the growth of Group 3 Medulloblastomas, the Taylor lab hopes to develop more effective treatments that can improve survival rates and reduce the chances of the cancer coming back.
In the future, we might be able to screen for these cells in children to catch potential tumors early, much like how gardeners might check their soil for the best conditions before planting. This proactive approach could help in preventing the cancer from developing in the first place. As these findings are further tested and developed, they hold the promise of not only better treatments but also preventive strategies that could save many lives. Incredible, right?!
Read Dr. Taylor’s paper here Early rhombic lip Protogenin+ve stem cells in a human-specific neurovascular niche initiate and maintain group 3 medulloblastoma and find the lab at Welcome | Michael Taylor’s lab at SickKids.




